60 y/o male with Shortness of breath
CBBLE UDHC SIMILAR CASES




Right foot ulcer
 Right forearm lesion
Right forearm lesion

Left leg lesion before treatment.

Left foot after treatment
Vitals on admission:
ECG: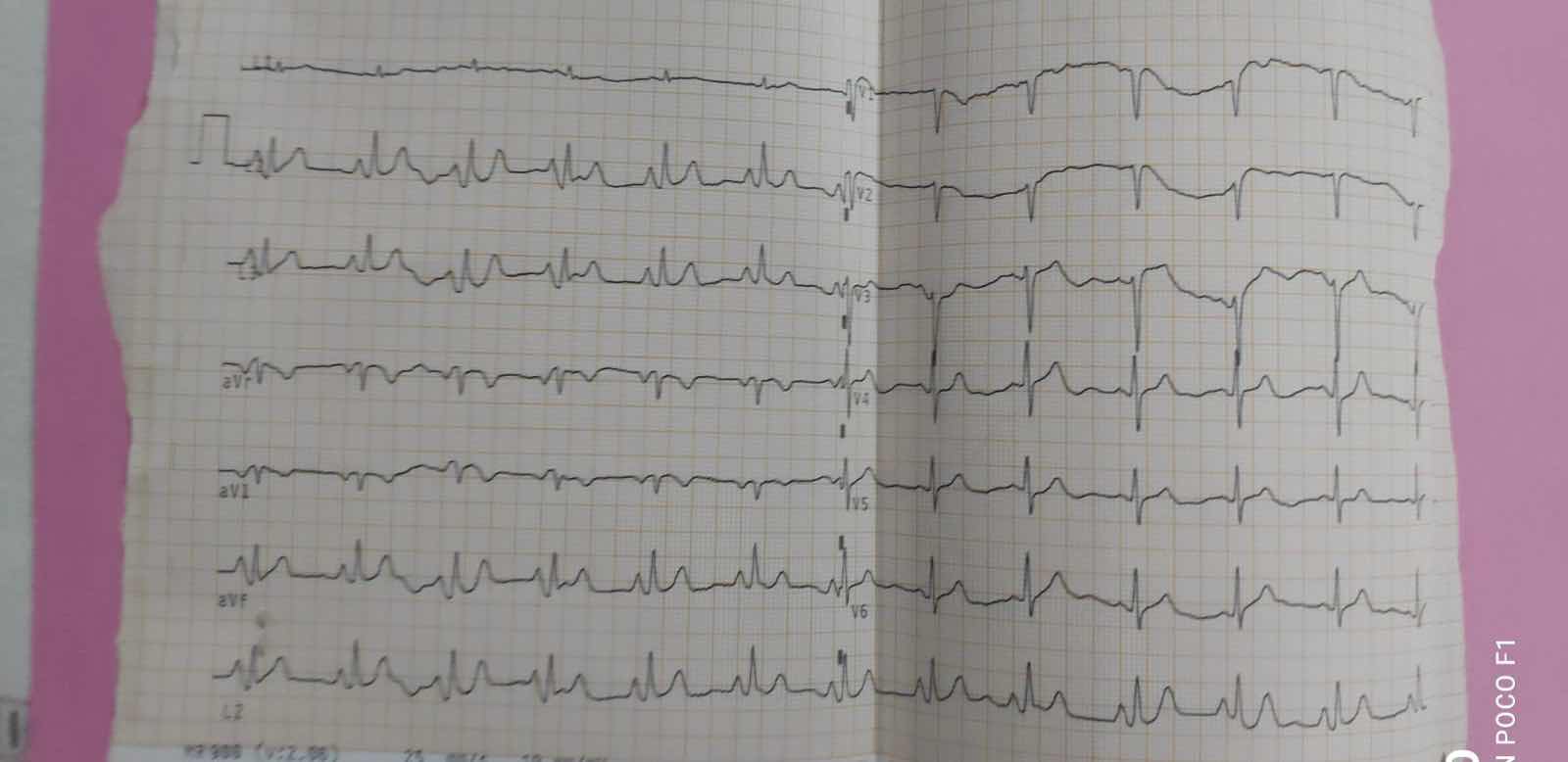
Chest X ray:

USG abdomen:

This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
A 60 year old male came to casuality with chief complaints of:
- Exacerbation of shortness of breath since 4 days
- Edema of right foot upto ankle since 4 days
History of presenting illness:
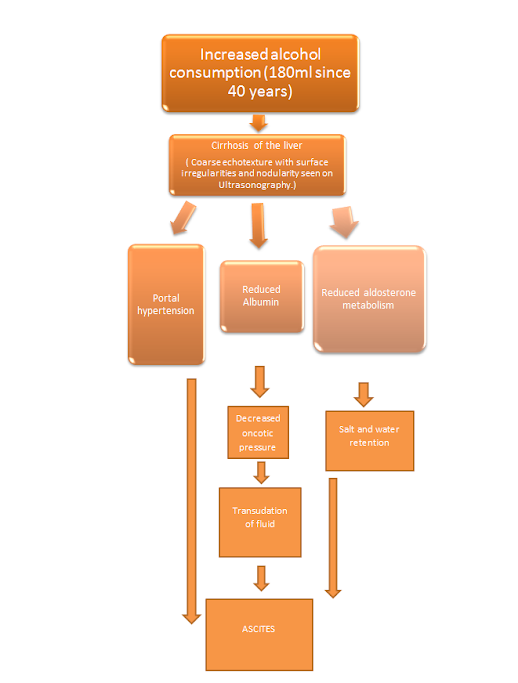
Patient was apparently asymptomatic 4 days back when he experienced a sudden exacerbation of Shortness of breath (grade III to grade IV). Patient complains of shortness of breath even at rest. His attenders say his shortness of breath exacerabated on drinking 90mL of whiskey 4 days back.
Patient complained of redness and edema of right foot upto ankle with a bullous lesion which was ?aspirated and was put on IV PIPERCILLIN- TAZOBACTUM, the redness has now subsided.
He was diagnosed with Bronchial asthma 10 years back, for which he used ?rotahaler twice a day for 5 months and then discontinued. He reports usage of Tab. Betnesol whenever he felt even slightly out of breath. His son reports frequent over consumption of these tablets.
5 years back, he had bouts of productive cough for 3 weeks and fever. He was taken to a local hospital where he was diagnosed with Tuberculosis. They opted for treatment from a Private hospital from where he took medication for 6 months but skipped a few doses in between and was irregular.
At the age of 25, he suffered right sided hemiplegia due to ischemic stroke for which he took treatment for 15 days at a local hospital.
At the age of 31, according to his wife, he suffered from high grade fever for which he was given ?medication and was advised to not consume alcohol.
But he consumed alcohol that night and then experienced dysarthria.
He was a coolie by occupation 15 years ago but stopped working due to shortness of breath.
No history of haemoptysis, COVID 19 infection, or reduced Urinary output.
Personal history:
Diet: mixed
Appetite: normal
Sleep: adequate
Bowel and bladder movements: regular
Addictions: consumes tobacco in the form of “chutta”, almost 10 per day, everyday until 4-5 days.
Consumed alcohol everyday about 45ml till 1 week back.
General examination:
The patient is conscious, coherent and cooperative.
Icterus present.
There is no pallor, cyanosis, clubbing, koilonychia or lymphadenopathy.
Right foot ulcer
Left leg lesion before treatment.
Left foot after treatment
Vitals on admission:
PR: 110 bpm
BP: 110/70 mmHg
RR: 40
SpO2: 99% at 4L O2
CVS: S1 S2 PRESENT
Respiratory system examination: BAE +
Diffuse rhonchi heard
Intercostal retractions present.
CNS: E4V5M6
P/A: soft and tenderness present in right hypochondrium.
Investigations:
ECG:
Chest X ray:
USG abdomen:
CBP:
Hb: 11 gm
TC: 10,900
N/L/M/E: 76/15/7/2
Plt: 6.10
D-DIMER: 970
LFT:
TB: 0.65
DB:0.20
AST: 14
ALT:11
TP: 5.8
Albumin: 2.8
RFT:
Urea: 35
Creat: 1.0
Uric acid: 2.4
Na: 141
K: 3.9
Cl: 102
Diagnosis:
Acute exacerbation of COPD with PAH with ?PE with right lower limb cellulitis and post TB sequelae.
Treatment:
1. Neb. DUOLIN-6th hourly , BUDECORT- 8th hourly, MUCOMIST- 4th hourly.
2. INJ. PIPTAZ 4.5g TID
3. INJ. PAN 40mg OD
4. INJ. DERIPHYLLIN 1 Amp BD
5. INJ. HYDROCORTISONE 100mg BD
6. Tab. SILDENAFIL 25 mg BD


Comments
Post a Comment