Medicine Blended Assignment (October)
I have been given the following cases to solve in an attmept to understand the topic of 'Patient clinical data analysis' to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis and coem up with a treatment plan.
Below are my answers to the Medicine Assignment based on my comprehension of the cases.
"57 year old man with jaundice, pedal edema and abdominal distension since three years and bleeding gums since three days"
https://swathibogari158.
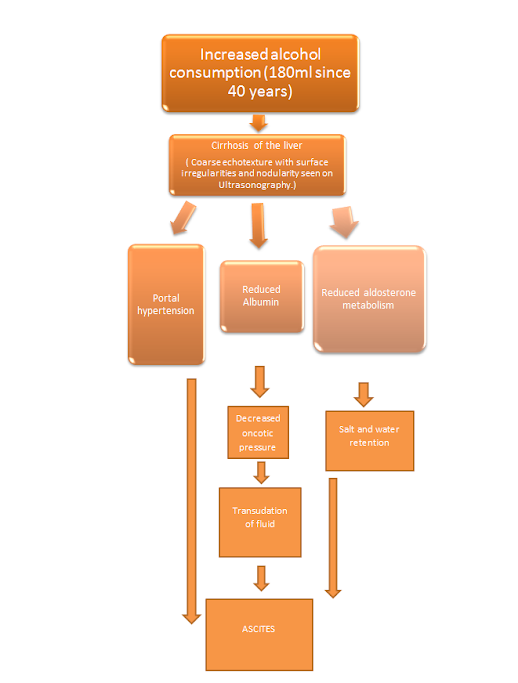
1) What is the reason for this patient's ascites?
Ans. This patient has the following features:
History
- Presenting complaints of Jaundice (icterus seen on sclera)
- Bilateral Pedal edema (pitting type) extending to knees and abdomen.
- Past history of consumption of 180mL whiskey everyday since 40 years
- Asterixis, constructional apraxia, forgetfulness and depression since 1 month.
- Black stools.
- Investigations show: Hypoalbuminemia (1.4 albumin) , Elevated Total and direct bilirubin,Elevated alkaline phosphatase and increased APTT and PT.
- Elevated serum creatinine and urea.
- Coarse echotexture with surface irregularities and nodularity seen on Ultrasonography.
Ans. The patient developed bipedal lymphedema (symmetrical) so a systemic pathology can be suspected. Here, Hypoalbuminemia and salt and water retention due to liver cirrhosis is the cause for bipedal lymphedema.
"Baddour and Bisno (1985) postulated that bacterial toxins which were ‘pooled’ in insufficiently drained lymphatic tissue contribute to the systemic symptoms found in some patients with cellulitis, complicating lymphoedema." (1)
3) What was the reason for his asterixis and constructional apraxia and what was done by the treating team to address that?
Ans.
2. Fluid restriction <1.5litres/day : to get rid of the fluid overload state.
Salt restriction <2.4gms/day
"There have been no studies on the benefits or harm of water restriction on the resolution of ascites. Most experts agree that there is no role for water restriction in patients with uncomplicated ascites. However, water restriction for patients with ascites and hyponatraemia has become standard clinical practice in many centres." (3)
3. Inj augmentin 1.2gm IV/BD: efficacy of 87.2%. It is being used to treat cellulitis. (4)
4. Inj pan 40 mg IV/OD
5. Inj zofer 4mg IV/BD
6. Tab lasilactone (20/50)mg BD: a diuretic combinatio used for treatment of fluid overload state
"Significant changes in BP were observed 1 week after initiation of therapy and were sustained during the observation period of 1 year. 3. Supine and standing BP fell from 148.6+2.6/102.1 f 1.9 to 120.8 f 1.4/91.7* 1.2 and from 154.4 f 2.1/106.1 f 1.6 to 125.7 &-2.2/90.7 f 1.5 mm Hg respectively. 4. There were no changes in the concentrations of plasma glucose, lipids, uric acid and potassium. On the other hand, levels of plasma renin activity rose from 0.69 + 0.06 to 3.95 + 0.47 ng/ml/hr and urinary aldosterone excretory rate increased from 9.6 f 1.6 to 42.8 * 4.2 pg/day. 5. This study suggests that addition of spironolactone to furosemide improves the hypotensive potency and minimizes the metabolic and electrolyte alterations of the latter."(5)
7. Inj vit k 10mg IM/ STAT (more efficacy than oral vit K and improvement in clotting)
8. Syp lactulose 15ml/PO/BD : for reducing the ammonia levels and improving the symptoms of hepatic encephalopathy.
"Over a median follow-up of 14 months, 12 patients (19.6%) in the lactulose group developed overt hepatic encephalopathy as compared with 30 patients (46.8%) in the placebo group (P = 0.001). The authors concluded that lactulose effectively prevented the recurrence of overt hepatic encephalopathy in patients with cirrhosis"(6)
9. Tab udiliv 300mg/PO/BD
"Udiliv®, 300 mg twice daily was preferred dose due to known efficacy (73.39%), as standard of care (62.5%) and good tolerability (45.56%). There was reduction in healthcare visits, inpatient hospitalization and days off work, within 4 weeks of treatment initiation (P<0.0001)." (7)
10.syp hepameiz 15 ml/PO/OD
" In conclusion, oral administration of lactulose or L-ornithine - L-aspartate to Mexican patients with cirrhosis and hyperammonemic encephalopathy significantly reduced serum ammonia levels in study groups and additionally improved mental status parameters, number connection test, asterixis scores, and EEG activity in the group receiving L-ornithine-L-aspartate." (8)
11.IVF 1 NS slowly at 30ml/hr
12. Inj thiamine 100mg in 100mlNS /IV/TID
13.strict BP/PR/TEMP/Spo2 CHARTING HOURLY
14.strict I/O charting
15.GRBS 6th hourly
16.protein x powder in glass of milk TID
17. 2FFP and 1PRBC transfusion
SECOND CASE
A 54 year old male with cough,abdominal tightness,pedal edema and diarrhea.
https://sainiharika469.blogspot.com/2020/09/hello- everyone.html?m=1
- After AST returns to less than two times the normal upper limit, Rifampicin can be restarted with or without ethambutol.
- After 3-7 days, Isoniazid maybe added, subsequently after checking AST levels.
- If symptoms recur, then the last drug added should be stopped.
- Fever which spikes at night
- Generalized weakness
- Sputum was found positive.
- Increased Neutrophil count points to an Active Pulmonary tuberculosis.
- Thromocytopenia
- Hazy opacities seen on Chest X ray.
- CT shows fibrocavitary lesion in right lung.
- Patient looks emaciated and has anemia which signify the severity of tuberculosis.
- Hepatic cirrhosis
- Chronic Pancreatitis
- Tuberculosis
Efficacy:" Fasting blood sugar (FBS) was found to improve in both groups but the percentage change in Mixtard group (14.5%) was more than Actrapid group (6.26%)" (11)
Inj PAN 40 mg IV/OD
Inj optineuron 1 amp in 100 ml NS Iv/bd
ATT to be with held
Syp lactulose 15ml HS
Protein powder 3 to 4 scoops in 1 glass of milk or water QID
Stop all OHA s
Grbs charting 6th hrly
Strict I/0 charting
High protein diet 4eggs daily : It has 79.7% efficacy.
ORS sachets in 1 litre of water
Bp charting hourly
Inj PIPTAZ 4.5gm/IV/bd stat - - --> TID
Vit k 10 mg Iv OD for 5 days
Temp BP PR monitoring 4th hourly
IVF - 1 DNS @50ml/hr
Nebulisation with salbutamol and mucomist 12th hourly.:
Inj thiamine 100 mg in 100 ml NS IV TID.
47 year old man with bipedal edema since one year and abdominal distension since one month
1) What will be your further approach toward managing this patient of nephrotic syndrome? How will you establish the cause for his nephrotic syndrome?
Ans. The patient should be started on diuretics and a low sodium diet and owing to his high cholesterol levels he should be started on statins.
A spot urine protein (161) so high indicates renal tubular damage. This is an indication for renal biopsy.
The accepted treatment in most cases of nephrotic syndrome is:
- Salt and fluid restriction
- Loop diuretics
- ACE inhibitors or ARBs
Electron microscopy should be done to determine the type of glomerulopnephritis.
-Drug history should be taken to look for drug induced nephrotic syndrome.
-Antinuclear antibodies and Complement C3 levels should be checked.
2) What are the pros and cons of getting a renal biopsy for him? Will it really meet his actual requirements that can put him on the road to recovery?
Ans. Pros:
- It will give us a hint about the cause of nephortic syndrome.
- It will be helpful in deciding the treatment as immunosuppressive therapy is deleterious if no proper reason.
- Invasive procedure.
- Expensive.
- For most of the etiologies of nephortic syndrome in adults, there is no cure and only supportive treatment so it might not impact the treatment.
References:
1. https://www.woundsinternational.com/uploads/resources/content_11173.pdf
2. 2. http://www.ghrnet.org/index.php/joghr/article/view/1014/1257
3. 3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1860002/
6. 6. https://emedicine.medscape.com/article/186101-overview#a7
9. 9. https://bmjopen.bmj.com/content/8/8/e021943
10. 10. https://gut.bmj.com/content/68/Suppl_1/A125.2
11.11.
https://pdfs.semanticscholar.org/c450/b34ed48123f3893520fdc353655599ceb5e6.pdf
12.




Comments
Post a Comment