Trio of Paraparesis cases
Diagnosis of a case begins right from when a patient enters the clinic,more so in cases of paraparesis . Many things which are probably unsaid by the patient are "given away" by the patient's gait, ability to walk or drag his leg. Lets explore on how to evaluate a patient with paraparesis.


The following structures are generally involved in causing paraparesis:
Upper motor neuron lesion: Cerebral cortex
Brainstem
Spinal cord (axons travelling upto ventral horn)
Lower motor neuron lesion: Anterior horn cell
Nerve
Neuro- muscular junction
Muscle
I've been given these three cases data here https://medicinedepartment.blogspot.com/2020/05/case-based-online-learning-assignment.html?m=1 to solve in an attempt to understand the topic of paraparesis.
CASE I:
I will be writing about his complaints in order of priority and what I thought of after reading the complaint. This way I'll be able to put across to the reader what goes on in my mind to come to a conclusion.
1. Weakness of lower limbs ,which is bilateral, since 20 days. (Chief complaint)
- Onset : Insidious
- Gradually progressive
- Weakness started in proximal region 2 YEARS back and later progressed to distal region
Thoughts: So this tells us that the weakness was chronic since it has been progressing since 2 years and as it is bilateral, we can call it paraparesis. Here we should clarify that paresis means loss of motor function partially.
It is also important to differentiate between weakness and fatigue as they are used interchangeably often.
To differentiate we have to determine whether there is a loss of muscle strength? or there is a feeling of general weariness, vague loss of energy and lassitude? The former hints at weakness and the latter fatigue. Interestinlgly, there are also medical conditions which cause both weakness and fatigue, for eg, Myasthenia gravis, Hypothyroidism. So we have to obtain a history carefully while differntaiting between the two as well as not exclude on due to the presence of another.
Now, it started in the proximal region and progressed to the distal area. This gives us a hint that it might be a type of muscular dystrophy.
2. Bilateral non pitting edema in the lower limbs.
Thoughts:Since it is non pitting type, we have to suspect a condition affecting the thyroid or lymphatic system.
And since its bilateral we can think of : i) Gravitational
ii) Usage of any sterioids or NSAIDS
iii)Lymphedema (any inflammatory conditions, infections or obesity?)
iv) Pre tibial myxedema
So here I want to ask a couple of more questions:
a) Do any of his daily activities involve standing for a long time?
b) Does the edema subside on rest i.e. maybe as soon as he wakes upin the morning?
c) Is he on any drugs? and can he be considered obese?
3. Difficulty in squatting position and getting up from squatting procedure.
Thoughts: Lets think of all the strcutures involved in getting up from a squatting position.
- Knee joint : arthritis? But isnt he too young for that? Apparently there is a type called Juvenile Idiopathic Arthritis.
To exclude it we need to ask questions like : Are his joints swollen?
Is there stiffness in his joints, especially in the morning?
Is there any difficulty or pain in moving the joint?
It also makes me think of rheumatoid arthritis but mostly the finger or wrist joints are effected and it's mostly be associated with fever or weightloss.
- Muscles of the leg,thigh, buttocks: might be due to wasting of the muscles or dystrophy?
- Muscles of hand and
- Cerebellum: any lesions or cerebellum? we can exclude this as the cause if he can stand up and maintain his balance. From the video we can see that he is able to walk and maitian balance.
So we suspect a problem with either the knee joint or the muscles.
To differentiate we get the following tests done: a)blood tests
b) EMG or NVC
c) Muscle or nerve biopsy
4. Difficulty of wearing and holding chappals.
This is a sign of distal muscular weakness.
5.Bilateral calf hypertrophy seen.
Thoughts:
- Now this is a classical sign of X-linked muscular dystrophies like Duchenne Muscular Dystrophy and Becker Muscular Dystrophy.
- Calf muscle hypertrophy is also seen in Pompe's disease(type 2 glycogen storage disorder due to acid maltase deficiency). Proximal muscle weakness, calf mucle enlargement and respiratory muscle involvement is usually seen. But absence of overt respiratory muscle involvement is not enough to exclude Pompe's disease.
- Hoffman's Syndrome,whcih is rare form of hypothyroid myopathy also presents as proximal muscle weakness and pseudohypertrophy of calf muscles. Pseudohypertrophy is when there is accumulation of glycosaminoglycans in the muscle.
- I found another interesting case of Sarcoglycanopathy which aso presented with calf muscle hypertrophy and proximal weakness of lower limbs.
So we need the following tests: a) Acid Maltase activity in leukocytes(chromogenic assay)
b) Muscle biopsy to look for vacuoles staining periodic acid schiff positive or muscle destruction and look for level of dystrophin or absence of delta sarcoglycan staining.
c) Creatinine Kinases levels and genetic testing to check for mutation in dystrophin gene.
d) Complete thyroid profile.
6. The patient has a high stepping gait.
seen in this video https://youtu.be/3VVH7w3rWSM.
Thoughts:
High stepping gait is usually due to a foot drop which is cauded by damage to common peroneal nerve.
It could be due to a motor neuron disease, neuromuscular disease or herniation of disc causing pressure on L5.
7. On examination of the motor system:
- Power in both the limbs : 4/5
- Reflexes: initially reduced in both the limbs and when repeated it was found that reflexes were absent.
- Sensory system and tone are normal.
Thoughts:
Since reflexes are redcued and then found absent, we loaclize the lesion to be a Lower Motor Neuron Lesion.
Hence now we narrow down to disorders of either Anterior horn cell, nerve, neuro-muscular junction or Muscle.
8. On investigation,
- Urea, creatinine, Uric acid ,phosphorus and chloride elevated.
These elevations reflect muscle destruction. High levels of uric acid and phosporus may also indica
te hypothyroidism.
Also high levels of urea,uric acid, creatinine, phosphorus and chloride shows that the kidney is becoming inefficient as it is unable to excrete them appropriately.
- Elevated lymphocyte count.
Denotes an infection or inflammatory state.
- Albumin and pus cells found in urine.
This indicates damage or healing along the urinary tract right from the kidneys to the urethra.
- Muscle biopsy: shows chronic inflammatory cells, connective tissue with adipocytes and blood vessels. There is also evidence of atrophy or necrosis of muscles.
Final thoughts: Based on the above conclusions, it is very much likely that the underlying pathology is of the muscles.
Hence, I suspect:
- Duchenne's muscular dystrophy: but the pateint should've presented earlier( childhood) with the symptoms.
- Becker's Muscular dysttrophy: this is similar to DMD, but the patients may present later in life and symtoms arent as severe.
- Limb Girdle Muscular Dystrophy
I would like to request for:
- Thyroid profile to exclude Hoffman's syndrome and hypothyroidism in this patient.
- Acid Maltase activity in leukocytes to exclude Pompe's disease.
- To look for absense of sarcoglycan in the muscle biopsy to exclude Sarcoglycanopathy
- Genetic testing and Western Blot.
Anatomical location: Muscles of the lower limbs. Even further we can say the short arm of X-chromosome is involved.

Treatment:
Pharmacological treatment:
- Steroids like Deflazacort and Prednisolone have been used as they have shown to increase muscular strength in patients with Becker's.
- "Gentamicin and Ataluren are expected to increase Dystrophin production by 21%" But studies showing no improvement on usage of the drug are also present.
- Vitamin D supplements are also of help as the patients are prone to pathological fractures.
Non Pharmacological treatment:
- Physiotherapy with early goal of stretching the tight muscles and later on providing the patient with assistive devices.
- Counselling the patient and his parents about the progression of the disease.
- Occupational Therapy
CASE 2
This is a case of a 23 year old male with the following complaints:
1. Weakness in the both the lower limbs since 5 days.
Acute onset of weakness generally makes us think of any Trauma to spinal cord or nerve compression? Thrombotic event? Transverse myelitis? Guillian Barre syndrome?
2. Vomiting (non projectile) since 5 days.
- I looked into causes for lower extremity weakness presnting with vomitting and found an interesting case of Thyrotoxic Periodic Paralysis here : https://journals.lww.com/em-news/fulltext/2018/10000/quick_consult__symptoms__extremity_weakness_and.14.aspx
But to confirm this we will require a thyroid profile, and we will have to look fro clinical signs like enlargemnt of the thyroid gland, proptosis andif any tremors are present.
3.Gluteal abscess since 5 months (operated on, 5 months back as well) and Scrotal abcess since 20 days.
- 2 instances of abcesses made me think of an immunodeficiency like : Diabetes Mellitus? HIV? Tuberculosis? Any chronic usage of steroids? Any carcinoma? Alcoholism?
- Taking an abscess biopsy is essential to find out what type of bacteria is causing the abscess.
4. History of multiple sexual partners
This made me look into all the venereal diseases which could cause weakness of the lower limbs:
- Human T-cell lymphotropic Virus: he has only 3 symptoms which could point towards this virus those being vomiting, paraparesis and frequent infections (being abscessses).
- Syphillis: Erbs parapelgia, which is spastic paraplegia is seen. But neurosyphillis usually takes about 10-20 years to present.
- HIV: I'm more inclined towards HIV now, that I have two pointers but there is no history of fever or diarhhoea which are very common symptoms of HIV
- Genital herpes: the patient does not have genital sores or any other symptoms pointing towards herpes.
- Hepatitis-B Associated Myelopathy
b) Detection of p24 antigen for HIV
c) HbsAg and Hbs antibodies
5.On examination,
- He has hypotonia in the lower limbs. (LMN lesion?)
- Babinski sign positive in right and left lower limb. (UMN Lesion?!)
- Superficial reflexes are present on both sides.
- Deep tendon reflexes:
Tricep, bicep reflexes are normal whereas jaw jerk is slight.
Ankle clonus is present on the right side. (UMNL?)
Right side gives me a predominant Upper Motor Neuron Lesion picture.
On the left side: Biceps, triceps and Jaw jerk are slight others being normal.( LMNL?)
Here I had major questions and made me look into conditions with both UMN & LMN lesion characteristics. I found that Demyelinating disorders like Multiple sclerosis. The more cases of Multiple Sclerosis I read, I realized that no two people present with the same symptoms. So for excluding Multiple sclerosis we need to get a couple of tests done like:
Spinal Tap : and look for antibodies
MRI
Evoked Potential Tests
A few Spinal Cord injuries also lead to UMN AND LMN .
- T3 – L3
- Upper limbs: normal
- Lower limbs: UMN
- L4 – S2
- Upper limbs: normal
- Lower limbs: LMN
Reference:
https://medatrio.com/upper-motor-neuron-lower-motor-neuron-lesions- Hence, Here we need to look for history of any trauma sustained. SO could there be a trauma in both the areas i.e. T3-L3 and L4-S2 or maybe an extension?
*I also a read a couple of articles which suggest that during the initial phase of an Upper Motor Neuron Lesion there would be flaccid limbs and loss of Deep tendon reflexes. So maybe the patient is in the inital stage. So he has to be reviewed a week later to see if there is any spasticity.
6. In the investigations done:
- Raised SGOT but normal SGPT ( isolated SGOT raise suggests that there isa a damage to one of the organs containing the enzyme such as liver,kidney,muscles, heart or brain.) I did think of Hepatitis B due to his sexual history and Hepatitis B associated Spastic paraplegia. So looking for HbsAg and Hbs Antibodies is pertinent now.
- There is also raised Alkaline phosphatase. There could be two causes for this either a problem with the liver or a bone related disorder or a vitamine D deficiency or if he was on any anti inflammatory or antibiotics. So a thorough drug history is required.
- Raised ESR and 15% lymphocytes whereas the normal lympocyte percentage should be between 20 and 40%. I attributed the raise in ESR to the abscess but I also doubted whether I can consider infection to be the cause since the lymphocytes are low, so I would like to know the neutrophil,eosionophil and basophil percentage as well.
- Imaging done revealed:
- significant enhancement which represents meningeal enhancement or exudates and following lesions in mri with multiple nodules in pulmonary apices suggest of pulmonary kochs and disseminated tuberculosis.
Here, I was surprised to find tuberculosis in the patient although, the immunocompromised state that I had expected would be present in the patient presented itself. This goes on re-iterate how diseases present uniquely in people.
 |
| Here I felt as though the space between the L4 and L5 vertebrae has been reduced. Which made me think of Nerve root compression due to a spinal cord injury. I was inclined to finding a spincal cord injury as I has suspected above when I saw symptoms of both UMNL and LMNL. |
Thoughts: Right Lower limb has symptoms of UMNL so could it indicate a lesion in the left medial area of cerebral cortex or the anterior paracentral lobule to be specific?
And left lower limb has LMNL so could it be due to the nerve compression by the L4-5 and hence a radiculopathy? or One could also suspect Pott's paraplegia, as the patient has disseminated tuberculosis, extensor plantar respsone and ankle clonus."Tuberculous spondylitis is also pretty comoon in the developing countries."
Or is it just the umnl in it's initial phases?
- Pharmacological: The patient should be started on Anti tubercular therapy and should be encouraged for subsequent follow ups to assess the efficacy of the treatment
- Non Pharmacological: The patient should be encourage to take physiotherapy for improvement of the weakness in the legs.
CASE 3
The symptoms of the 18 year old male patient in order of priority are :
1.Weakness in the lower limbs since 1 month along with pain in the calves while walking.
Peripheral neuropathy? Arterial or nerve claudication like sciatica?Cauda Equina syndrome?Electrolyte imbalance?Guillian Barre Syndrome? Juvenile Myositis?Spinal cord injury?Any Thyroid condition?
We need to ask if the pain increases in the night for narrowing down.
2.History of difficulty in standing from sitting position,climbing stairs and holding chappal
This points towards stiffness of joints which may be because of any arthritic condition, maybe Juvenile arthritis? Herniated disc?
3.History of thinning and wasting of muscles
Lower motor neuron lesion?
4.History of fever

- There is more than 1 degree change in 24 hours and it doesnt touch the baseline, so it coudl be remittent fever which is caused by upper respiratory tract viruses,mycoplasma, legionella.
- Upper respiratory Tract infections like the Flu have been infamous for causing Infectious Myositis.
- After knowing about the history of fever, weakness and pain, I also came across an article in whichLyme disease is known as 'The great mimicker" of Fibromyalgia,Arthritis,Multiple Sclerosis and Neuropathy.
- GBS can also present with fever and progressive weakness of limbs and loss of reflexes.
Tests required: A) ELISA for antibodies to Borrelia Burgdorferi. It requires very specific
testing.
B) Check for history of any Upper respiratoy tract infection in the past.
C) Nerve conduction studies and CSF anlysis to be done for confirming
GBS.
5. Personal History
We come to know that the patient works on the tractor and also consumes alcohol twice weekly.
Now, when we think of working with a tractor, it consists of sitting on a vibrating surface for a long time. This causes an upward force towards the pelvis and Lumbar spine. There is an upward force and then it becomes normal,here are repetitive cycles of this force which causes vibration. This makes the individual prone to mechanical stress on the Lumbar nerves or the Lumbosacral plexus. Hence a nerve compression is likely.
 |
| Source: http://krishi.icar.gov.in:8080/jspui/bitstream/123456789/3293/1/Seating%20discomfort%20for%20tractor%20operators%20%7D%20a%20critical%20review.pdf |
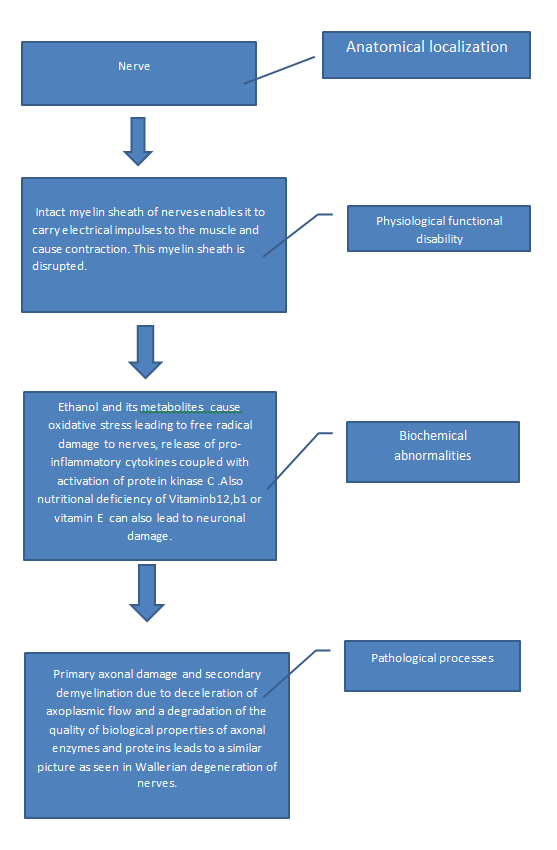
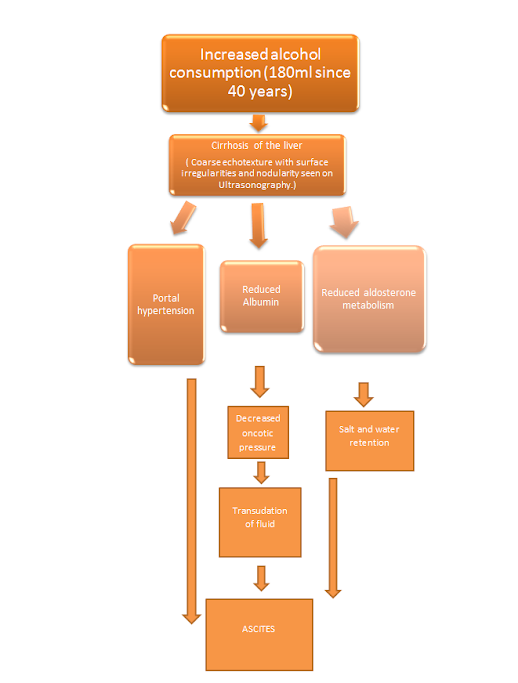
- Chronic alcohol consumption causes malnutrition due to poor absorption of nutrients such a Thiamine, Vitamine B12, folic acid which are essential for neuronal health.This might also cause anorexia.Chronic alcoholism is when >4 drinks are consumed on an occasion or >14 drinks per week.
*Not every tractor driver develops a complication but since our patient has a history of twice a week alcohol consumption which might lead to release of free radicals coupled with mechanical stress form the tractor puts him more at risk of developing a peripheral neuropathy following a nerve compression.
6. Examination
- Pallor is present and he has microcytic and hypochromic anemia. I was expecting a megaloblastic anemia cosidering B12 deficiency is prevalent in alcoholics. Microcytic hypochromia is commonly due to iron deficiency anemia, thalassemia, anemia due to chronic diseases, lead posioning or sideroblastic anemia.
Now, lead toxicity has been shown to cause paraparesis especially due to chronic lead toxicity "has been implicated in the pathogenesis of Amyotrophic Lateral Sclerosis". Being involved in farming, might have exposed him to harmful pesticides containing lead.
Or it could be due to decreased iron absorption due to alcohol consumption as Chronic alcoholics prefer drinking to having meals.
Tests required: a) A blood test to detect for Lead. Gums can also be looked for blue lines.
b) Iron indices like Transfeeric saturation, ferritin and Transketolase levelsin RBC can be checked to detect any thiamine deficiency.
- He exhibits hypotonia in both the lower limbs and deep tendon reflexes are absent.This is characteristic of a lower motor neuron disease and contributes to our hypothesis of a peripheral neuropathy.
After a day's time he has shown decrease in the upper arm power, which indicates spread to the upper limbs as well which is a characteristic of Peripheral neuropathy.
- On further examination, he was found to have scabies. And he doesnt seem to find it pruritic. Interestingly, Norwegian scabies which occurs most commonly in alcoholics doesnt cause itching. So maybe we can attribute it to the alcohol consumtion?
- His thyroid profile showed decreased T3 level and a possibilty of thyroid myopathy was considered.
- Further, a Nerve Conduction Test was conducted, which showed Bilateral common peroneal and sural axonal neuropathy. Hence it does give us some sort of confirmation of a peripheral neuropathy.
Treatment
- Pharmacological treatment: a) For Scabies, he should be advised to take scabies and listen to the instructions of application carefully. The family should be advised to take the treatment and necessary precautions too.
b) For peripheral neuropathy,Over the counter pain medication acetaminophen is advised or corticosteroid injections can be taken.
- Non pharmacological treatment: a) Alcohol consumption should be restricted. CAGE questionnaire maybe used to determine if the individual consumes too much alcohol.
b)Ergonomic cats or splints maybe used to provide support to the part which feels uncomfortable.
c)Physiotherapy can be advised to better handle the weakness of legs.
d) Prolonged sitting on tractors should be avoided. There should be intervals of 'no vibration' to avoid stress on the nerves. Maintainence of a proper posture on the tractor should also be advised.
By studying this topic I realise how important it is consider every possibility of a disorder to occur, also taking into account the rare presentations. Hopefully, this will make me more competent in making a diagnosis and help me save a human's "precious podes".
References:
https://hitesh116.blogspot.com/2020/05/12may-2020-elog-medicine-intern.html?m=1st
https://srianugna.blogspot.com/2020/05/hello-everyone.html
https://srianugna.blogspot.com/2020/05/hello-everyone.html
https://wikem.org/wiki/Lymphedema
https://kidshealth.org/en/teens/juv-rheumatoid-arthritis.html
https://www.healthline.com/health/muscle-atrophy#diagnosis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3440798/
https://emedicine.medscape.com/article/313417-treatment#d9
https://www.researchgate.net/publication/313729042_Calf_Muscles_Hypertrophy_in_Sarcoglycanopathy
https://rarediseases.info.nih.gov/diseases/9645/human-t-cell-leukemia-virus-type-1
https://www.telegraphindia.com/health/lyme-and-other-tricky-tick-diseases-in-india/cid/1684530
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3370340/
https://www.medicinenet.com/what_is_norwegian_scabies/views.htm
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3370340/


Comments
Post a Comment