Fighting for breath
Hello. I am a 4th year MBBS student who's trying to enhance her competency in the field of medicine.
http://medicinedepartment.blogspot.com/2020/05/re-case-based-online-learning.html to solve in an attempt to understand the topic of "Breathlessness".
First case
Identification: The patient is a 35 year old male.
On having a glance at the patient's history, I felt that the patient was previously healthy till he develpoed a viral fever,which tuned out to be malaria. So we need to be thorough with the history to know if :
- Did the preceding illness cause his breathlessness or are they unrelated?
- Did the drugs used to cure the fever show any side effects in the patient? If yes, then what made him more prone to develop them?
Some more questions I have :
- What type of malaria was it?
- Was his recovery smooth?
I ask these questions to rule out any skeletal or cardiac complications caused due to malaria or the anti-malarial drugs.
"the inflammatory characteristic of Plasmodium parasites increases cytokines levels (such as tumour necrosis factor, TNF) in combination with the formation of highly damaging free radicals , which could be considered as a potential important mechanism of damage and muscle weakness." (1)
His complaints in order of priority are:
- Shortness of breath
- Pedal edema
Now, lets delve into the details of the patients history:
1.Shortness of breath
- Onset: Sudden and from 2 weeks
- Class: initially NYHA 3, with treatment reduced to NYHA 2
- Progress:
- Continuous or intermittent: continuous
- Associated symptoms :
*Generalized weakness (Neuromuscular disorder? or could it be a side effect of malaria or the drugs used?)
Here, we need to ask:
*What was the relieving factor of the paroxysmal nocturnal dyspnea?
- Was it coughing or was it simply hyperventilation?
This will help us know whether it is due to an underlying cardiac or respiratory cause.
*Is there any diurnal variation of the weakness the patient is experiencing?
To exclude Myasthenia Gravis(increased weakness in the evenings).
Things to observe in a patient to understand the severity:
- Is he unable to speak?
- is he sweaty?
- Is he Pale?
First we need to determine whether the shortness of breath is Acute or Chronic?
- It seems to be ACUTE as it is since 2 weeks. But we cannot rule out the chronic causes as occasionally patients with Chronic progressive dyspnea present after a few days itself.
Some examinatory findings to get more information about the shortness of breath:
- Respiratory system: Right sided early inspiratory crepts in the Infrascapular area.
So it is essential to rule out any COPDs.
- Jugular Venous pressure is raised (Indicates increased right atrial pressures,so a high input or valve problem?)
- Post prandial blood sugar level raised (this could either mean diabetes mellitus or impaired glucose tolerance as his fasting blood sugar is 102)
There are two classifications for the causes of Shortness of breath:
i) Based on the pathophysiology

ii) Based on Organ involved
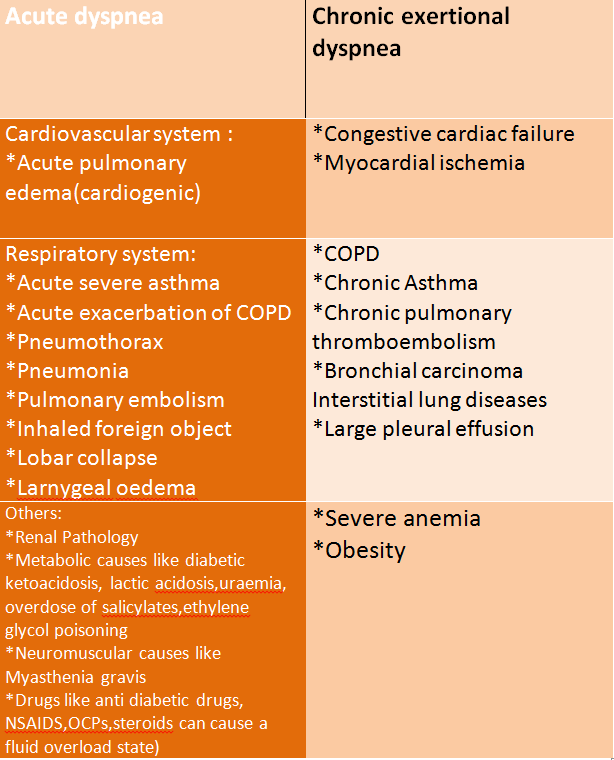 |
| Source: Davidson's Principles and Practice of Medicine |
--->Now we know that, There is an acute Shortness of breath associated with Paroxysmal Nocturnal Dyspnea and raised JVP.
- So I suspect a cardiac pathology along with a respiratory disorder.
- I would also like to exclude a few life threatening conditions,such as :
- Pulmonary edema: Chest X ray, Blood test for Arterial Blood Gas concentrations and Brain Natriuretic Peptide levels in blood to check for a cardiac cause of Pulmonary edema.
- Acute coronary syndrome: ECG and cardiac markers (Troponin-T &-I, Creatinin Kinase-MB)
- Cardiac Tamponade: 2-D echocardiography, Muffled heart sounds, raised JVP and low blood pressure.
- Pneumothorax: A prompt chest X ray, we should also look for family history of pneumothroax and history of any COPD.
- Suggested Investigations:
b) Chest X-ray
c)Check for Brain Natriuretic Peptide levels and cardiac markers.
2. Pedal edema
- Bilateral pedal edema since 2 weeks
- Pitting type (Renal? Cardiac? Hepatic?Severe malnutrition?)
- Extending upto knees (grade 2)
- Progressing in nature
The pedal edema here is CHRONIC as it lasted for more than 72 hours.

Causes of Chronic Bilateral pedal edema:
- Venous insufficiency (more common in persons above 50years and he doesnt seem to have any pain on walking or itching in the legs)
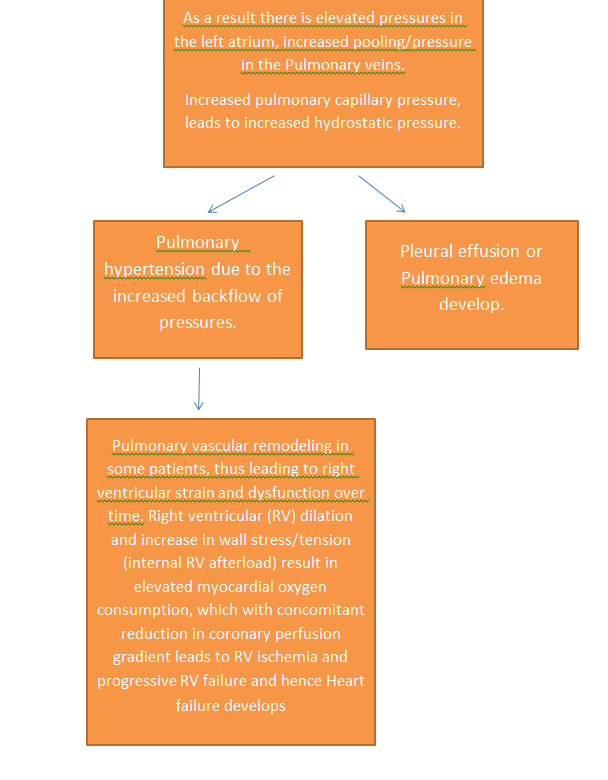
- Pulmonary hypertension
- Heart failure
- Idiopathic edema
- Lymphedema
- Drugs
Premenstrual edema(since he his a man, we can exclude this cause)Renal disease(nephrotic syndrome, glomerulonephritis)Liver disease- Secondary lymphedema (secondary to tumor, radiation, bacterial infection, filariasis)
-
Pelvic tumor or lymphoma causing external pressure(No history of weight loss, or any pain in the pelvic region) - Dependent edema (We need to ask questions like, does the swelling reduce in the morning, that is after sleeping?)
- Diuretic-induced edema (Drug history needs to be checked, especially the drugs he used for the betterment from Grade 3 NYHA to Grade2)
-
Preeclampsia -
Anemia(The patient has a haemoglobin level of 15.2)
I think it could either be
- pulmonary hypertension
- or Heart failure
- or edema due to drugs.
-->Pulmonary hypertension and heart failure have similar symptoms.
Either we have to differentiate between the two or we can think of one as a consequence of another.
Tests needed:
a) Echocardiogram: to check the blood pressure in the pulmonary arteries and also to calculate the ejection fraction.
b) ECG: to detect left ventricular hypertrophy or right ventricle under strain.
c)Optional can be: Chest X ray and Ct scan of lungs.
Questions:
- Is the pedal edema associated with tenderness? (to rule out of Deep Vein Thrombosis)
- A proper drug histroy of the patient needs to be obtained. Any calcium channel blockers,prednisone, diabetes medication or anti inflammatory drugs used?
- We also need to ask for history of Sleep Apnea as it is an often underlooked cause of pulmonary hypertension.
At the end of history I suspect:
--> I should also mention that the patient has a history of smoking and alcohol consumption occasionally.
But we need some more history about the smoking habits and a chest X ray to confirm a COPD.
Investigatory findings:
1. Electrocardiogram

Interpretation:
a) Rhythm: seems to be irregular. (Arrhythmia)
b) Rate: about 100 bpm.
c) Fragmented ORS complex: in V2 and V3 (NOTCHED S)
in V1 (notched R) (indicates a Premature ventricular complex)
This indicates Myocardial scar & conduction disturbance.(2)
Myocardial scar could mean:
- Previous myocardial infarct (he does'nt have history of a previous attack)
- Myocarditis (Viral infection is the most common cause [3] of myocarditis and since he had a viral infection episode a month ago, we can suspect this etiology)
- Cardiomyopathy (myocarditis caused by a viral etiology usually causes dilated cardiomyopathy)
"Profibrotic cytokines like TNFα, IL1β, IL4, IL17, and transforming growth factor β1 (TGFβ1) are believed to initiate remodelling during acute myocarditis that results in the appearance of cardiac fibrosis/scar tissue several weeks or months later."[6]
So to confirm a myocarditis causing a dilated cardiomyopathy we need:
a) Cardiac magnetic resonance, plays an increasingly important role, although
b) Endomyocardial biopsy is still considered a gold standard for diagnosis.[4]
2. Jugular venous pressure interpretation
Seen here: https://drive.google.com/file/d/1Gr2xuU5bcPUbNmQaPjVIavwn1m-FK7gr/view?usp=drivesdk
Prominent 'v' wave : as seen in the lower half of the neck.
Indicates:
- Tricuspid regurtitaion
- Right ventricular failure (this could also be thought of as a consequence of myocarditis)
Atrial Septal Defect(Usually present earlier)
Causes of Tricuspid regurgitation:
- Pulmonary hypertension
- Cardiomyopathy
- Heart failure
Injury to chest(no history)Infection: Rheumatic fever and infective endocarditis can affect the tricuspid valve.(can be ruled out due to no fever of bacterial origin and history of attacks of sore throat.)Congenital conditions: Conditions present at birth can cause tricuspid valve failure. These include:- Ebstein’s anomaly, where the valve isn’t formed normally
- Marfan's, an inherited disorder of the connective tissue. (WOULD'VE POSED A PROBLEM EARLIER)
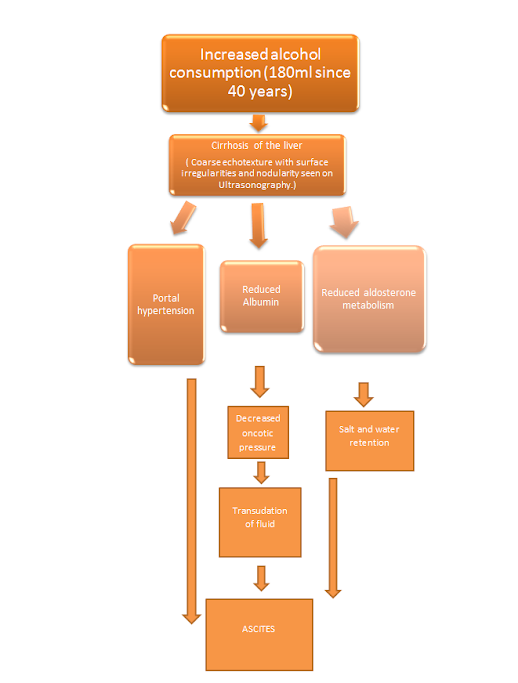
3.Ultrasonography interpretation
- Right moderate pleural effusion
- Mild ascites
- Grade 1 fatty liver
Causes of pleural effusion(transudate type):
- Congestive Heart Failure
Hepatic cirrhosis(would be seen on USG)Nephrotic syndrome(No facial puffiness,oliguria or proteinuria)Chronic Kidney Disease(no facial puffiness,frothy urine seen)
-->Right pleural effusion+Mild ascites+Pedal Edema = indicates a fluid overload state.
Now this fluid overload state can be caused by:
- Heart Failure
Cirrhosis(he has grade 1 fatty liver as seen in USG)Kidney failure(Creatinine,urea and uric acid levels are normal)Nephrotic syndrome( no facial puffiness,no oliguria and no proteniuria)
Now lets look for some confirmatory findings:
1.2D ECHO:
- EF-27%,
- IVC dilated(2.3cm)not collapsing
- mild TR+
- severe MR+,
- trivial AR+
- dilated all chambers
- global hypokinesia,
- severe LV dysfunction
- mild PAHT,
- no MS/AS,
- no PE/LV clot
Hence we can pursue as diagnosis the following:
a) Dilated cardiomyopathy as a result of myocarditis.
Reasons to think so:
- Symptoms of dyspnea and pedal edema.
- History of fever of viral cause
- Fluid overload condition(pleural effusion,mild ascites and oedal edema)
- ECG findings
- Dilation of all chambers on 2D ECHO, as suspected.
- We also have to consider that the patient was treated of his fever with Chloroquine.SO we need to acertain whether there was a side effect of the drug.
"Chloroquine and related drugs are highly tissue-bound (volume of distribution [Vd] = 150–250 L/kg) and are eliminated very slowly from the body. The terminal half-life of chloroquine is 2 months, and that of hydroxychloroquine is 40 days" [5]
This proves that the drug might still be present in the patient and that we cn still acertain any toxicity.
"Toxic dose. The therapeutic dose of chloroquine phosphate is 500 mg once a week for malaria prophylaxis or 2.5 g over 2 days for treatment of malaria. Deaths have been reported in children after ingesting one or two tablets—doses as low as 300 mg; the lethal dose of chloroquine for an adult is estimated at 30–50 mg/kg."[5]
" Severe chloroquine overdose may cause convulsions, coma, shock, and respiratory or cardiac arrest. Quinidine-like cardiotoxicity may be seen, including sinoatrial arrest, depressed myocardial contractility, QRS- and/or QT-interval prolongation, heart block, and ventricular arrhythmias. Severe hypokalemia can occur with either chloroquine or hydroxychloroquine and may contribute to arrhythmias."
We have observed:
- Depressed myocardial contractility in the patient.
- Ventricular arrhythmia in the patient.
We can also check for Hypokalemia in the patient.
-->But to confirm a case of viral myocarditis it is Imperative to get a cardiac magnetic resonance (non invasive) or a endomyocardial biopsy.
b) Pulmonary hypertension
- complaint of pedal edema
- We required a 2-D ECHO to differentiate or relate heart failure and pulmonary hypertension as causes for Pedal edema.
- And once 2-D ECHO was done: we found that There was mild Pulmonary arterial Hypertension.
c) Tricuspid regurgitation
- Due to the prominent 'v' waves seen in JVP.
- It fits in the progression of heart failure.
Treatment:
1)Pharmocological:
- Angiotensin-converting enzyme (ACE) inhibitors. These medications, such as enalapril (Vasotec), captopril (Capoten), lisinopril (Zestril, Prinivil) and ramipril (Altace), relax the blood vessels in your heart and help blood flow more easily.
- Angiotensin II receptor blockers (ARBs). These medications, such as losartan (Cozaar) and valsartan (Diovan), relax the blood vessels in your heart and help blood flow more easily.
- Beta blockers. Beta blockers, such as metoprolol (Lopressor, Toprol-XL), bisoprolol and carvedilol (Coreg), work in multiple ways to treat heart failure and help control arrhythmias.
- Diuretics. These medications, such as furosemide (Lasix), relieve sodium and fluid retention.
"Hemodynamically stable patients with DCM and symptomatic heart failure may benefit from angiotensin-converting enzyme inhibition or angiotensin receptor blockade. In euvolemic patients with DCM, β-adrenergic blockade may improve LV function, heart failure symptoms, and decrease inflammation. Patients who have persistent heart failure symptoms despite optimal management with angiotensin and adrenergic pathway inhibition may benefit from aldosterone antagonists, such as eplerenone or spironolactone. Diuretics should be used to optimize intravascular volume."[8]2) Surgical:
- Mitra clip: Mitraclip Is Performed Through A Small Hole In The Groin – No Open Heart Surgery Is Required.
"The COAPT trial was based out of the United States and randomized 614 patients with symptomatic HFrEF and moderate-severe MR to MitraClip and optimal medical therapy versus optimal medical therapy only. Patients with Stage D HF or severe LV dilatation >7 cm were excluded. Implementation of optimal therapy including CRT was supervised by the core committee."
"In COAPT, 98% of patients achieved a successful reduction in MR, and MitraClip in combination with medical therapy demonstrated a statistically significant reduction in HF hospitalization (number needed to treat of 3.1) and a reduction in 2-year all-cause mortality."[9]
Prognostic factors:
1. IVC dilated and not collapsing is a bad prognotic factor.
"A dilated IVC without collapse with inspiration is associated with worse survival in men independent of a history of heart failure, other comorbidities, ventricular function, and pulmonary artery pressure."[7]
2. Severe Mitral regurgitation is a bad prognostic factor in this case.
"Secondary or functional MR is commonly seen in HF with reduced ejection fraction (HFrEF) patients and is a poor prognostic marker." [9]
At the end, The questions remain:
1.What was the dosage of Chlorquine given to him? What was the treatment he recieved for improvement from Grade 3 NYHA to grade 2?
2. Why is there presence of early inspiratory crepts in this patient with pleural effusion, when early inspirtaoy crepts indicate Chronic Obstructive Pulmonary Disorders?
3. Why did pleural effusion occur and not pulmonary edema when mechanism of rise of backflow pressures from left atrium is the same in both?
4. Why was no chest X-ray taken to better understand the lung pathology?
5. How was a severe Mitral reguritation hidden? There was no systloic murmur neither any characteristic ECG changes?
Learning from conversations:
[30/05/20, 6:30:21 AM] Shri Valli: Good morning sir. I just wanted to know what Early inspiration crepts in the infra scapular region indicate. I read two conflicting articles sir: 1. https://www.sciencedirect.com/topics/medicine-and-dentistry/crackle Sir here it says, early inspiratory crackles are due to COPD, bronchiectasis or heart failure as in non fibrotic conditions less tension is required to open the airways. "In a study by Pürilä and colleagues,86 the crackles of pulmonary fibrosis began at 45% of inspiration, whereas those of nonfibrotic lung conditions were heard earlier: COPD at 25%, bronchiectasis at 33%, and heart failure at 37% of inspiration.86 This suggests that more tension is required to open individual airways in fibrosis than in lungs with secretions or edema. As inspiration progresses, radial traction on airway walls increase until the small airways pop open" 2. https://www.medscape.com/viewarticle/712242_5 "Early inspiratory crackles, however, imply significantly decreased FEV1/ forced vital capacity caused by broncho obstructive disease."
[30/05/20, 9:22:10 AM] Dr. Biswas Sir Gen Med: In simple terms they would be sounds generated in the proximal part of the airway anatomy maybe in the larger airways while they end inspiratory would be likely to be more distal in the alveoli?
[30/05/20, 10:18:21 AM] Shri Valli: Okay sir. So can we also conclude anything about the underlying pathology? Like could it be a non fibrotic cause in case of early inspiratory crepts?
[30/05/20, 1:00:18 PM] Shri Valli: Sir. Early inspiratory crepts indicate a problem with the large airways. But when the crept are basal, can't it indicate a small airway problem? [30/05/20, 4:42:29 PM] Dr. Biswas Sir Gen Med: Basal would indicate a problem with the area of the lung there. Likely the lower lobes. The other way to distinguish between large airways and small airways is by pitch where the pitch will be higher (fine creps) in smaller airways as they vibrate well and lower (coarse creps) in larger airways
[30/05/20, 4:46:32 PM] Shri Valli: So sir in pulmonary edema what are you most likely to hear?
[30/05/20, 4:47:35 PM] Shri Valli: <attached: 00000146-PHOTO-2020-05-30-16-47-34.jpg>
[30/05/20, 5:01:04 PM] Dr. Biswas Sir Gen Med: Fine crepitations
[30/05/20, 5:01:39 PM] Dr. Biswas Sir Gen Med: Yes ventricular premature complexes
[30/05/20, 5:02:59 PM] Shri Valli: Okay sir thank you! [30/05/20, 5:03:23 PM] Shri Valli: Sir, it isn't mentioned whether the crepitations
are fine or coarse. 🙈 [30/05/20, 5:17:54 PM] Dr. Biswas Sir Gen Med: Ask the original poster to mention 👍
[30/05/20, 5:19:24 PM] Shri Valli: Okay sir. Thank you! [30/05/20, 7:13:04 PM] Shri Valli: <attached: 00000154-PHOTO-2020-05-30-19-13-04.jpg> [30/05/20, 7:13:20 PM] Shri Valli: Is it of any significance or is it just his posture? [30/05/20, 8:38:18 PM] Dr. Biswas Sir Gen Med: Posture [30/05/20, 9:21:59 PM] Shri Valli: Okay sir.
Second conversation:
[29/05/20, 6:13:16 PM] Shri Valli: Good evening Maam! Maam do we know what medication did the 35 y/o patient take for malaria?
[29/05/20, 6:13:43 PM] Rashmita Rao Kims PG Medicine: It wasnt documented but may be chloroquine
[29/05/20, 6:14:09 PM] Shri Valli: Okay Maam. And what treatment did he take for improvement in NYHA grade?
References:
1) 1) https://malariajournal.biomedcentral.com/articles/10.1186/s12936-016-1577-y
2) 2) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3443879/
3) 3) https://www.myocarditisfoundation.org/research-and-grants/faqs/causes-of-myocarditis/
4) 4) https://pubmed.ncbi.nlm.nih.gov/22927087/
5) 5) https://accessmedicine.mhmedical.com/content.aspx?bookid=391§ionid=42069865
6) 6) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5813801/
7) 7) https://pubmed.ncbi.nlm.nih.gov/16504642/
8) 8) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2770911/
11






[01/06/20, 10:39:20 AM] Shri Valli: Sir I just had a conversation with the DCM patient sir.
ReplyDelete[01/06/20, 10:39:37 AM] Shri Valli: He told me that he used drugs related to malaria for 10 days
[01/06/20, 10:40:18 AM] Shri Valli: And his dosage was twice a day.
He apprently doesn't have the prescription or any remaining strip of the medicine.
[01/06/20, 10:40:57 AM] Shri Valli: He remembers being able to work for 2 months after the fever and medication.
I. E in Oct Nov
[01/06/20, 10:41:45 AM] Shri Valli: From December 20th, he faced weakness.
And his pedal edema seemed to be less in the morning and progressed during the day time.
[01/06/20, 10:42:41 AM] Shri Valli: On asking his present condition, he says he feels weak and attributed it to the heat.
On asking about his activity, he says he's at home and is feelings dyspneic even on walking in the house, on waking up and before going to sleep.
[01/06/20, 10:43:12 AM] Shri Valli: He's also taking his anti diabetic medication regularly and is keen to come for his check up next week.