63 y/o Male with SOB and haemoptysis
CBBLE UDHC SIMILAR CASES



No history of head injury, palpitation, chest pain, no h/o valvular disorder.
Past history:

Old Adverse Drug Reaction lesions over thigh.




This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
A 63 year old right handed male, Supervisor of department of adult education by occupation, came on 20/3/22 with complaints of
- Shortness of breath and
- haemoptysis since 19/3/22 7 PM.
History of presenting illness:
Patient was apparently asymptomatic one day back, and then developed shortness of breath, sudden in onset. It subsided after a while and patient went to sleep.
After he slept, his son noticed that there was drooling of saliva and there were 3 blood stained sputum on the bedsheet.
No history of head injury, palpitation, chest pain, no h/o valvular disorder.
No h/o diagnosis of tuberculosis, no h/o exposure to STD.
Not diagnosed with Diabetes Mellitus, epilepsy, tuberculosis or asthma.
There was no h/o waxing and waning.
Past history:
2011: The patient went for a regular health check up and was diagnosed with Hypertension and started on TAB. TELMA CH 40mg.
On 7th August 2011, At 12AM the patient had one episode of vomitting and then slept but next day morning, he didn’t wake up at his usual time. When his son went to wake him up, he noticed that he was unable to move his right upper and lower limb and had slurring of speech.
He was taken to a local hospital and then to NIMS, was diagnosed with Stroke secondary to Left Thalamic bleed and received treatment from 8-28th august. He underwent physiotherapy sessions as well and completely recovered in three months.
He went for regular checks ups, after first three months of treatment and then twice 6 monthly.
2011 to 2014- he worked well and did his own chores.
In 2014, he retired.
Jan 21, 2021:
At 7 PM, he was watching TV and he tried getting up from his chair and fell down. He developed weakness of his Left upper and lower limbs and there was deviation of mouth towards right side.
At 9:30PM, he was taken to hospital where he received treatment for 1 week and was advised physiotherapy.
After he came back home, he could walk only when supported by 2 people and was fed food with a spoon.
After a month, he himself tried to pick up mug from the bucket, tried combing his hair and used to try standing up.
On Feb 2022, he was watching TV and seemed very confused and dull, so was taken to the hospital next day where CT was done and they were told that there were no new developments and prescribed medication.
The patient developed Adverse drug reaction to ? Escitalopram . He developed papules over his trunk, back and thighs. He also developed cheilitis and had discharge, which hardened as crust over his eyes.
Old Adverse Drug Reaction lesions over thigh.
He was taken to the hospital for this and was given a lotion and CIPROFLOXACIN eye drops.
ON 6th March, 2022: the patient ate and 30 ministers later went to bed and developed 4 episodes of tonic movements of the left UL and LL,each lasting for <5mins.
The patient also felt fullness of bladder but couldn’t pass urine. He experienced two such episodes per day, but the attender also says that he eventually could pass urine.
On reaching the hospital (the patient was supported on two sides and made to sit in a car) his SpO2 was found to be 90% and was found to have fever. After a chest x ray, he was diagnosed with Right Lower lobe pneumonia, was given nebulization.
On 12th March, he was discharged.
Post discharge status: the patient was not oriented to place and time. He could recognize all his family members and could walk with support. He only communicated if he had a strong urge to micturate.
On 19th March, he did his physiotherapy and went to sleep. His attenders noticed that he was drooling saliva and that he was 3 bouts of blood stained sputum. On 20th March morning, when he washed his mouth, the water was blood stained initially but later normal.
Now, he couldn’t walk inspite of support from two people, he felt weakness of his left upper and lower limb, he apparently couldn’t rest his feet on the ground, there was also up rolling of eyes, which resolved 25 mins later.
Personal history:
Diet: mixed
Appetite: decreased
Sleep: excess
Bowel and bladder movement: bowel movements regular(sometimes hard stools), decreased urination.
Addictions: used to occasionally drink 15 years ago.
Not a smoker.
General examination:
The patient is conscious, incoherent and uncooperative.
Pallor present.
No Icterus, cyanosis, clubbing, lymphadenopathy or edema.
Vitals on admission:
BP: 70\60—>90/60 mmHg
PR: 110 bpm
RR: 28/min
SpO2: 88% on RA and 98% on 10 L O2
CVS: S1 S2 +
RS: BAE +
CNS: E4V3M4
Motor system:
Tone: R. L
UL. N. Hypotonia
LL. N. Hypotonia
Power: R. L
UL. 5/5. 0/5
LL. 5/5. 0/5
Reflexes: R. L
B. +++ +++
T. +. +
S. ++ ++
K. +++ +++
A. Couldn’t elicit
Babinski. B/L positive( dorsal fanning of toes)
Investigations:
20/3/22
ABG:
pH: 7.43
HCO3: 15.8
PCO2: 24.1
PO2: 103
Hb: 6.0
TLC: 10,700
N/L/E/M: 87/16/2/4
RBC: 2.2
PCT: 4.1
D-DIMER: 980
APTT: 32
BT: 2 min
CT: 4 min
PT: 16
INR: 1.11
MP: negative; blood for MP strip: negative,
dengue serology negative
ESR: 120
CRP: 1.2 mg/dl
Blood urea: 165
S. Creat: 1.5
Na: 143
K: 3.9
Cl: 99
TB: 0.6
DB: 0.2
AST: 20
ALT: 19
ALP: 60
TP: 4.3
Alb: 2.1
A/G: 0.97
CUE:
Alb/sugar: nil
Pus cells: 2-3
Epithelial cells: 1-2
Chest X-ray:
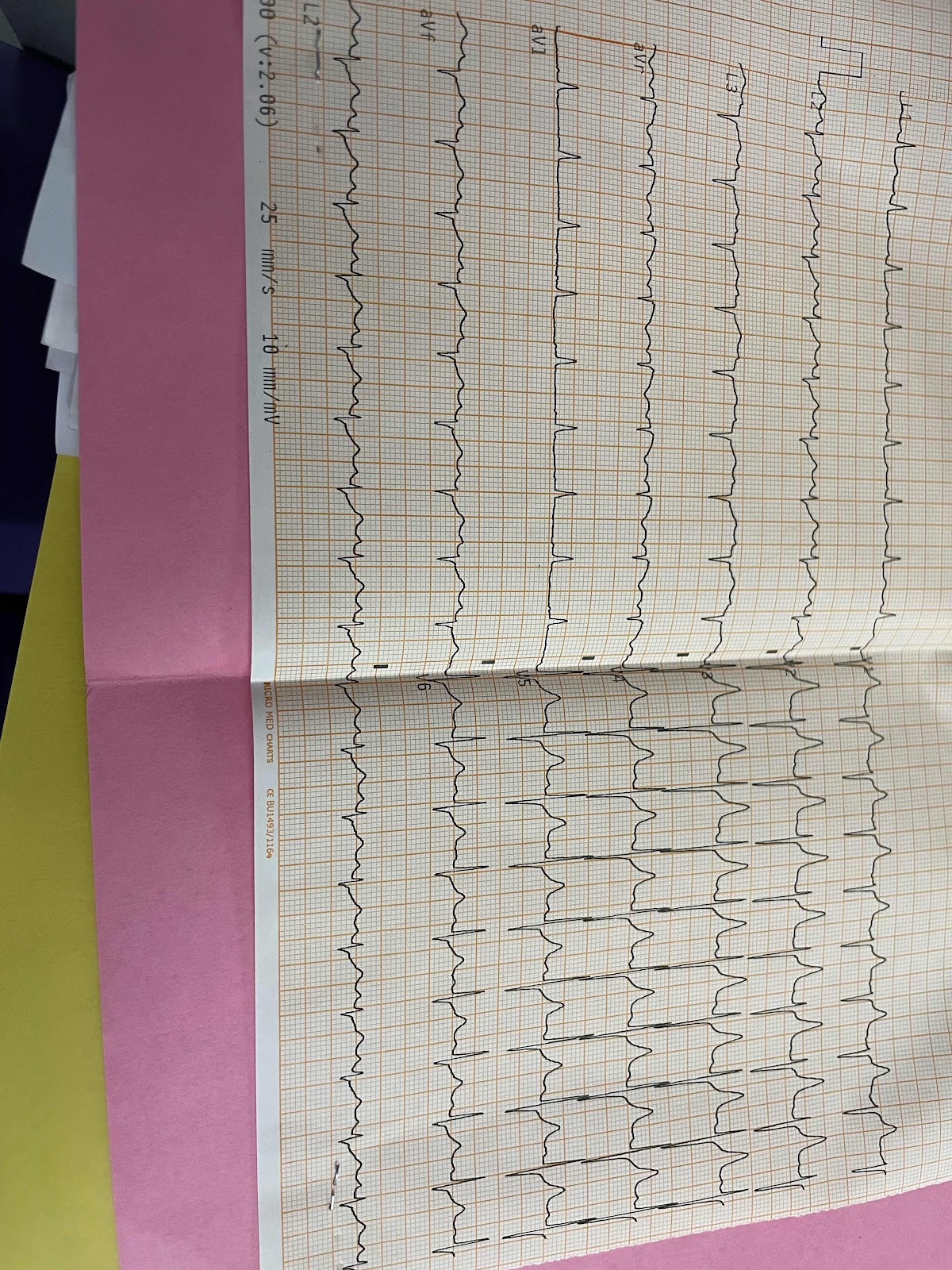
ECG:
CT brain:
Diagnosis:
Recurrent CVA with left hemiparesis
With history of Hypertension since 10years
With CVA episodes in 2011 (right hemiparesis) and 2021 (left hemiparesis)
Treatment:
1. IVF NS and RL at 75 ml/hr
2. INJ. NORAD at 6ml/hr to maintain MAP > 65mm Hg
3. INJ. MONOCEF 1gm IV BD
4. Tab. ECOSPORIN 150mg RT OD
5. TAB. CLOPIDOGREL 75mg RT OD
6. Tab. ATORVAS 40mg RT/OD




Comments
Post a Comment