Medicine blended assessment
I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and diagnosis with a treatment plan.
CASE:
1. Pedal edema
- Onset: insidious; on and off from 5 months back and progressive edema since 5 days.
- Bilateral pedal edema.
- Pitting type (Renal?Cardiac?Hepatic?Severe Malnutrition?)
- Progressive over a course of 1 week. Started in lower limbs and progressed to cause facial puffiness and abdominal distention. (facial puffiness hinting at renal cause? could aso be myxoedema?)
- Aggravating factors: Walking
- Relieving factors: on rest.
- Venous insufficiency (We'd require history of itching in the lower limbs,pain on walking, varicose veins)
- Heart failure
- Pulmonary hytertension
- Renal disease (likely,as facial puffiness is seen)
- Liver disease (abdominal distention is present)
- Secondary lymphedema
- Anemia
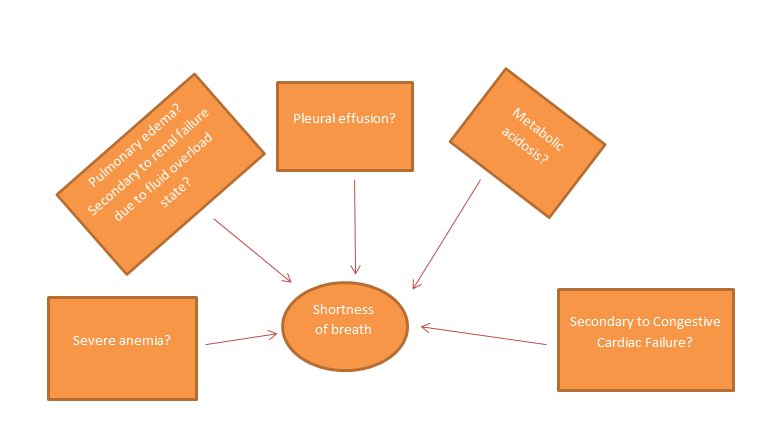
2.Shortness of breath
- Onset: sudden and from 5 months.
- Class: grade 3 initially but grade 4 since a week.
- Continuous or intermittent: Continuous
This Chest Xray shows:
- Blunting of cardiphrenic and costophrenic angles.
- Onset: sudden since 1 week.
- Non radiating
- Associated with: intermittent palpitations
- Most of the ESRD patients develop Congestive Cardiac Failure. This patient shows chest pain along with shortness of breath which can be caused by Heart Failure, bilateral pedal edema is also supportive. Congestive Heart Failure is one of the most common complications of ESRD so it is is highly suspected.
- Pulmonary complications such Pleural effusion and Pulmoary edema can also occur due to changes in pulmonary vascular permeability and increase in pulmoary capillary pressure.Interestingly, due to heart failure also ne can develop altered pressures leading to pleural effusion or pulmonary edema.
- Regular rhythm
- Rate: 100 bpm
- P waves present indicating sinus rhythm.

4. Past Medical History
- Diabetes Mellitus type 2 since 5 years.
- Hypertension since 1 year.
- Pallor is present. (Suggestive of anemia)
- Ulcer on right sole (foot ulcers are a common complication of uncontolled diabetes mellitus, so suggestive microvascular damage)
- Blood pressure : 180/80 mm Hg
- Per abdomen : distended

6. Investigations:
- Elevated urea (92mg/dl)
- Elevated creatinine (6.4mg/dl)
- Elevated uric acid (7.7.mg/dl)
- Low Calcium level (8.4mg/dl)
- High Phosphorus(6.6mg/dl)
- Low sodium (130mEq/L)
- Low potassium (2.9mEq/L)
- Microcytic hypochromic anemia evidenced on smear.
- Presence of Albumin +4 indicated. (This reflects large amount of protein loss, and is a marker of Renal damage)
- Presence of Pus cells
- Presence of Epithelial cells
- Presence of Red Blood Cells (this indicates glomerular bleeding)
- Blood pH is 7.19 (acidic)
- Partial pressure of CO2 is low (indicating compensated metabolic acidosis)
- Partial pressure of O2 is elevated. (indicating hyperventilation)
- Bicarbonate levels are low (indicating metabolic acidosis)
- Pain abdomen and no urine was passed.
- Respiratory rate has increased from 13 to 20cpm. (Maybe for compensation of metabolic acidosis but HCo2 injections were given)
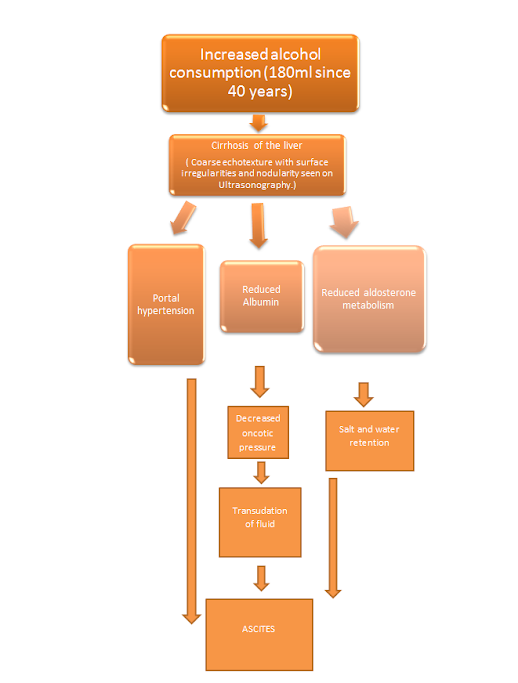
- Serum Albumin is found to be low (indcating Hypoalbuminemia)
- Blood pH is now 7.22 (still acidic but improved)
- Partial pressure of Co2 has increased to 22 but is still low.
1.inj.HAI according to sliding scale
2.t.OROFER xt bd
3.t.PAN 40 mg od
4.inj.LASIX 40 mg iv bd if systolic bp >110mmhg
- Shortness of Breath of sudden onset
- Raised Bp 170/90 mm Hg
- Metabolic acidosis
- Refractory anuria
- Worsening of fluid overload. But furosemide was given? Furosemide is a loop diuretic and it relieves fluid overload by causing diuresis but this woman has anuria so I think it worsened her situation.
"Renal hypoperfusion causes AKI, which may present itself with oliguria or anuria. Unfortunately, loop diuretics are accepted as ‘urine producers’ among physicians in ICUs and are often used. Therefore, under such conditions, the unnecessary use of loop diuretics may worsen renal blood flow contributing to AKI and worsen the clinical prognosis." (1)
- Lower doses of Diuretics are not effective to treat fluid overload due to nephrotic syndrome.
"In nephrotics, edema is often refractory to diuretics because of low plasma protein, depletion of the intravascular compartment, decrease in the protein-bound fraction of the diuretic in peritubular blood, and increase in tubular fluid. Thus, higher doses are needed." (2)
- Short duration of Furosemide maybe a cause.
"Diuretic resistance may be caused by decreased renal function and reduced and delayed peak concentrations of loop diuretics in the tubular fluid, but it can also be observed in the absence of these pharmacokinetic abnormalities. When the effect of a short acting diuretic has worn off, postdiuretic salt retention will occur during the rest of the day."(3)
--> Opthalmology referral showed moderate Hypertensive Retinopathy. (indicates uncontrolled hytertension)
On Day 4,
Arterial Blood Gas Analysis:
- The pateint shows improvement in blood pH to 7.35.
- The Partial pressure of CO2 has also improved.
Questions:
Other possible etiologies:
- Malignant hypertension causing Nephropathy
- As a part of cardiorenal syndrome?
The sequence of events according to me is:
2) What are the reasons for her:
Azotemia :
- This is biochemical abnormality in whcih there is accumulation of nitrogenous waste and creatinine in the blood.This is due to impairment of renal function of excretion of these waste products. In this case, there is oliguria due to damage to glomeruli and there is decrease in Glomerular filtration rate which leads to accumulation of creatinine and nitrogenous waste.
- Impairment of capillary circulation in the kidney due to edema and tubular obstruction from protein casts are also possible reasons for azotemia in nephrotic syndrome pateints.
Anemia:
Anemia in this patient is due to :
- Deficiency of erythropoietin.
- Reduced red cell survival.
- Reduced intake,absorption and utilization of dietary iron.
- Blood loss in the form of haematuria.
Hypoalbuminemia:
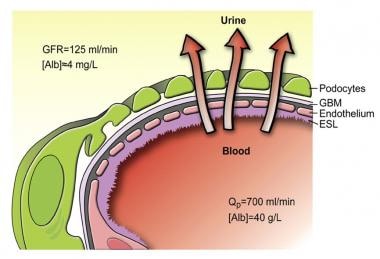 |
| Source: https://emedicine.medscape.com/article/244631-overview#a3 |
Acidosis :
- Acid base balance is maintained by excretion of acid by excretion of H+ ions and ammonium.In ESRD, there is decline in the number of functional nephrons which leads to retention of H+ ions, Impaired emmonia excretion and decreased tubular reabsoprtion of bicarbonate.
- Insulin deficiency also leads to acidosis as when the body is unable to utilize glucose as energy source, it uses amino acids and triglycerides.Due to lipolysis, there is a rise in level of glycerol and free fatty acids.
- Glucagon is also released due to iniabilty to utilize glucose, which stimulates conversion of free fatty acids to ketones. The major ketoacids produced, acetoacetic acid and beta-hydroxybutyric acid, are strong organic acids that create metabolic acidosis.
3) What was the rationale for her treatment plan detailed day wise in the record?
Particularly mention rationale and efficacy for some of the drugs administered such as oral and iv bicarbonate? When is iv or oral bicarbonate indicated and why is it contraindicated in certain situations?
- Efficacy of Sodium Bicarbonate in treating metabolic acidosis in ESRD:
"Patients supplemented with oral sodium bicarbonate are less likely to experience rapid progression of kidney disease."(4)"The relative risk for all-cause mortality in the second trial was 0.83 (95 % confidence interval, 0.68, 1.02) and renal replacement therapy was used less frequently in the bicarbonate group. These two broadly positive efficacy findings of the trial, however, are negated somewhat by the finding that bicarbonate therapy was associated with increased risk of hypocalcemia and hypokalemia requiring treatment (respective relative risks, 1.65 and 1.14). Data relating to any efficacious or deleterious effect on hemodynamic parameters was lacking. Overall statistical analysis revealed that certainty of the clinical efficacy of sodium bicarbonate was low." (5)
Indications of IV or Oral Bicarbonate:
- Cardiac conduction delays
- QRS prolongation (ex. tricyclic antidepressant poisoning)
- Metabolic acidosis
- Nebulized sodium bicarbonate is an excellent option to treat chemical injuries resulting from chlorine gas, especially within the pulmonary mucosa.
Contraindications:
- Due to rapid alkalotic effects, sodium bicarbonate is contraindicated in those with symptoms or laboratory values indicating metabolic or respiratory alkalosis due to the potential for exacerbation of symptoms.
- Due to its ability to alter acid-base balance and buffer pH, It can influence certain drug interactions such as with Antibiotics(Doxycycline, levofloxacin, minocycline, tetracyclines),NSAIDs/other related anti-inflammatory medications and Mesalamine, sulfasalazine. This is especially seen when both Sodium bicarbonate and these drugs are taken orally.
- The administration of sodium bicarbonate can exacerbate hypernatremia.
- Rapid or high dose administration of undiluted sodium bicarbonate may lead to decreased CSF pressure and intracranial hemorrhage.
2.syp.POTCHOLR 15 ml in one glass water tid: it contains Potassium chloride and is used to treat hypokalemia in this patient to prevent adverse effects of hypokalemia like arrhytmias and muscular spasms. Hypokalemia is a dangerous complication of ESRD which should be corrected.
3.w/h all OHA,anti hypertensives : To keep diabetes mellitus and Hypertension under control respectively.
Day 2:
1.inj.HAI according to sliding scale: Human Insulin (Regular) is gieven perhaps to gain better control of her uncontrollled diabetes, sliding scale means to adjust the dose of insuline according to pre meal glucose level.
2.t.OROFER xt bd : contains ferrous ascorbate and folic acid. Used to treat her Iron deficiency anemia.
3.t.PAN 40 mg od:
It is well known that PPIs indirectly elevate serum gastrin levels via a negative feedback effect. Interestingly, in type 2 diabetes mellitus (T2DM) animal models, it has been reported that PPIs improved glycemic control, probably via possible effects on augmenting both serum levels of gastrin and β cell mass. (6)
4.inj.LASIX 40 mg iv bd if systolic bp >110mmhg : diuretic furosemide is a short acting loop diueretic given to alleviate fluid overload.
Day 3:
1.inj.lasix 40mg iv bd
2.tab.dytor 20mg of po: now along with Furosemide, torsemide is also added as in ESRD patients, higher doses of diuretics are required to reduce fluid overload.
3.inj.HAI S/C according to sliding scale
4.tab.telma 40 mg od po->tab.nicardia 10 mg po/sos
Stopped telma : Angiotensin Receptor Blocker was stopped and switched with calcium channel blocker.
"Taking the RENAAL and IDNT trials together, the suggestion is that it is safe and effective to coadminister CCBs along with ARBs in the management of hypertensive type 2 diabetics with nephropathy.
Adding a CCB to an ACE inhibitor or an ARB helps in reaching goal BP, while preserving renal function in both diabetics and nondiabetics with proteinuria." (7)
5.tab.orofer ct bd po
6.inj.erythropoietin s/c twice weekly: due to inadequate production of erythropoeitin in this patient, these injections ahve been prescribed.
7.tab.nodosis 500 mg bd po: Sodium bicarbonate tablets to perhaps counteract the metabolic acidosis.
8.tab.shelcal ct po/op: to counteract the hypocalcemia in this patient secondary to ESRD.
9.syp.potcholr 15ml in one glass water tid
Day 4
Blood is transfused and an imrovement in Hb is seen to 8.4 mg/dl.
Day 5
1.Syp.lactulose 30ml bd : this laxative is given to relieve constipation in this patient.
2.protein x powder 2tbsp in one glass milk bd: to compensate for the lost protein via proteinuria.
3.inj.MONOCEF 1gm IV bd: antibiotic
4) What was the indication for dialysing her and what was the crucial factor that led to the decision to dialyze her on the third day of admission?
Ans. The indication to dialyse her was Overload with fluid refractory to diuresis.
The patient developed:
- Shortness of Breath of sudden onset ( The overload with fluid resistant to diueresis could cause pulmonary edema)
- Raised Bp 170/90 mm Hg
- Metabolic acidosis
- Refractory anuria
- Worsening of fluid overload. But furosemide was given? Furosemide is a loop diuretic and it relieves fluid overload by causing diuresis but this woman has anuria so I think it worsened her situation.
"Renal hypoperfusion causes AKI, which may present itself with oliguria or anuria. Unfortunately, loop diuretics are accepted as ‘urine producers’ among physicians in ICUs and are often used. Therefore, under such conditions, the unnecessary use of loop diuretics may worsen renal blood flow contributing to AKI and worsen the clinical prognosis." (1)
- Lower doses of Diuretics are not effective to treat fluid overload due to nephrotic syndrome.
"In nephrotics, edema is often refractory to diuretics because of low plasma protein, depletion of the intravascular compartment, decrease in the protein-bound fraction of the diuretic in peritubular blood, and increase in tubular fluid. Thus, higher doses are needed." (2)
- Short duration of action of Furosemide maybe a cause.
"Diuretic resistance may be caused by decreased renal function and reduced and delayed peak concentrations of loop diuretics in the tubular fluid, but it can also be observed in the absence of these pharmacokinetic abnormalities. When the effect of a short acting diuretic has worn off, postdiuretic salt retention will occur during the rest of the day."(3)
The fluid overload refractory to diuretics and persistent hypertension inspite of antihypertensives are crucial factors in deciding emergency dialysis.
5) What are the other factors other than diabetes and hypertension that led to her current condition?
- I think her Severe Anemia (Hb 6.4) played a role in her edema, shortness of breath and palpitations.
- Abdominal distention could also have lead to difficulty in breathing due to increased pressure on diaphragm and inhibiting it's efficient contraction. It is not a Huge factor but might have contributed.
- Hyperkalemia also contributes to breathing diffculties and palpitations.
- Malnutrition due to loss of proteins through urine can also contribute to her edematous state.
- Her Age,not that significant though.
"In T2DM patients, the prevalence of both eGFR and Albuminuria increase with age. "(8)
- The patient could survive upto 3 years.
"The median survival of dialysis patients with baseline HF has been estimated to be 36 months, in contrast with 62 months for those without baseline HF . Over 80% of ESRD patients who are recently diagnosed with HF are expected to die within only three years from the time of this diagnosis."(9)
- 5 year survival is possible too.
"The 5-yr survival in CHF was even worse: 12.5%In the study that compared different subgroups, the patients with diabetes and the elderly had worse outcome. " (10)
- A case study of a Mrs. A from Eastern Samar, Phillipines, suffering from ESRD due to diabteic nephropathy but aged 69years. She did not respond to any medications and died soon. (https://www.scribd.com/doc/13870941/Diabetic-Nephropathy-Case-Study)
- CHF patients progressing to dialysis- dependent renal failure had a grave prognosis: median survival time was 95 days, mean survival 444 days.(https://pubmed.ncbi.nlm.nih.gov/19626297/)
- Better Hyperglycemia control could lead to better outcomes:
" Although neither the Diabetes Control and Complications Trial (DCCT) in type 1 diabetes nor the UKPDS in type 2 diabetes showed a reduction in cardiovascular events with intensive glycemic control, a prospective, observational component of UKPDS revealed a continuous relationship between glycemic exposure and the development of HF with no threshold of risk, such that for each 1% (absolute) reduction in glycosylated hemoglobin (HbA1c), there was an associated 16% decrease in hospitalization for HF ( Similar findings also were reported recently in a large cohort study from the US ." (11)
- Better self care such as :medication adherence, glucose monitoring, dietary modification, physical activity, weight and stress management, restricted dietary sodium and fluid intake and symptom management
"In a small, qualitative meta-analysis, patients with DM and HF reported lack of knowledge, skill, and efficacy in integrating multiple self-care behaviors, which led them to prioritize some over others (eg, glucose monitoring, but not daily weights)."(12)
Newer Therapies:
- "trials using compounds that can break the covalent AGE cross-links, with their potential to reverse established disease, seem to be the most advanced. These agents that include alagebrium chloride (ALT 711; Alteon Inc., Parsippany, NJ), a stable derivative of N-phenacylthiazolium bromide , is under investigation for a range of potential indications that include DHF and diabetic nephropathy. Indeed, the findings of a small 23-patient DHF study were published recently showing that after 16 wk, alagebrium reduced left ventricular mass along with a trend to improvement in E/E′"(12)
- "In a recently reported pilot phase 2 clinical study, patients with type 2 diabetes and nephropathy were administered ruboxistaurin 32 mg/d along with continued ACE inhibitor and/or ARB for 12 mo, noting a significant decrease in albumin:creatinine ratio from baseline of 24% (P = 0.02) that did not change in the placebo group (−9%; P = 0.33) . Furthermore, estimated GFR fell over 1 yr in placebo-treated patients (modified Modification of Diet in Renal Disease −4.8 ± 1.8 ml/min per yr; P = 0.009) but not in the ruboxistaurin-treated group (−2.5 ± 1.9 ml/min per yr; P = 0.185)."(12)
- N-terminal Pro BNP levels: more than 100pg indicates heart failure.
- ECG and Echocardiogram can be used to check the pumping function of heart.
- Chest Xray
Intrabdominal and central venous line pressure elevation- Activation of Renin Angiotensin System
- Sympathetic overactivity
- Oxidative injury and endothelial dysfunction
- Injection Erythropoietin:
"low-dose weekly SC rHuEPO administration was a safe and effective method for maintaining the hematocrit value of the stable hemodiabysis patients who volunteered for this study. Weekly SC rHuEPO maintained hematocrit value as well as conventional IV therapy, " (14)
"The baseline hemoglobin level was higher in the rHuEPO group (9.9 +/- 1.15 g/dL vs. 9.3 +/- 1.41 g/dL, p = .02) as was the pretransfusion hemoglobin level (8.0 +/- 0.5 g/dL vs. 7.5 +/- 0.8 g/dL, p = .04). At day 84, patients receiving rHuEPO received fewer red blood cell transfusions (median units per patient 0 vs. 2, p = .05), and the ratio of red blood cell transfusion rates per day alive was 0.61 with 95% confidence interval of 0.2, 1.01, indicating a 39% relative reduction in transfusion burden for the rHuEPO group compared with placebo."(15)
- Tablet orofer which contains same components asPhosfomin
" A total of 56 patients, who were between 18-55 years of age, with hemoglobin (Hb) 6-9 g/dl and serum ferritin <15 mg/l also complying with the inclusion and exclusion criteria in the protocol were enrolled in the study after obtaining necessary approvals and informed consent. All were dispensed with Phosfomin-XT fixed-dose combination (FDC) of ferrous ascorbate (equivalent to elemental iron 100 mg) + folic acid 1.5 mg tablet once-daily after food for eight weeks. Patients were assessed at baseline and Weeks 2, 4, 6 and 8 for change in Hb level, clinical evaluation and target Hb achievement. Results: Baseline mean Hb was 08.39 ± 0.75 g/dl, which significantly increased to 9.76 ± 0.70 g/dl (16.3%) at Week 2 and further increased to 10.70 ± 0.70 g/dl (27.53%) at Week 4. At Week 6, it increased to 11.55 ± 0.67 g/dl (37.7%) and at Week 8, it increased to 12.53 ± 1.09 g/dl. Conclusions: The present study concludes that Phosfomin-XT (ferrous ascorbate, equivalent to elemental iron 100 mg + folic acid 1.5 mg) tablet should be preferred as first choice of oral iron salts to treat IDA due to positive effect on Hb value and superior tolerability." (16)
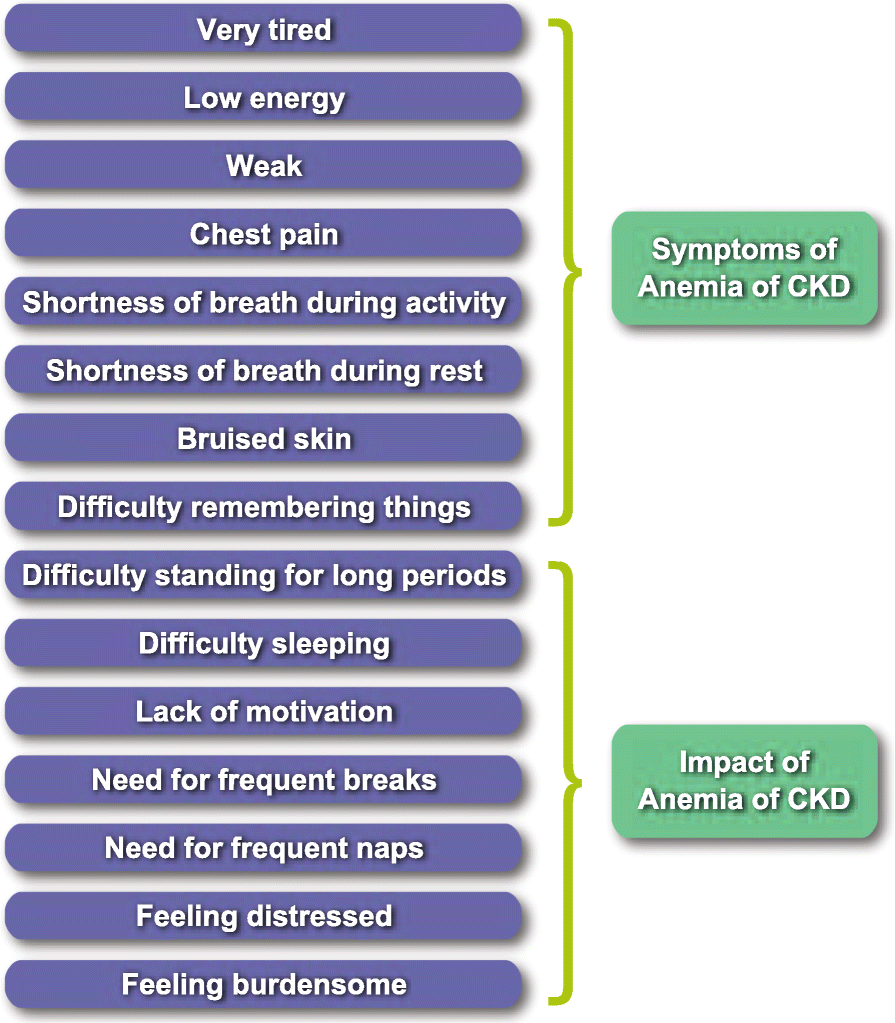 |
| Source:https://jpro.springeropen.com/articles/10.1186/s41687-020-00215-8 |
- Since it is based on patient reporting, It provides relevant questions to be asked and also provides insights of the patient.
- Some symptoms mentioned in the questionnaire like difficulty remembering things, difficulty concentrating, and restless legs were reported only after probing. This shows that providing a questionnaire makes it easy for the patient to mention all the applicable symptoms(which are mentioned in the questionnaire after rigorously collecting data from several CKD patients.)
- Also, this eliminates doubts of if a particular symptom is caused by CKD or another underlying cause. The patient can easily answer without having to think the symptom is irrelevant to anemia in CKD.
"English for Canada, UK, Australia, India, and South Africa are required. The original version of the instrument is US English." (17)"In parallel to Wave 2 interviews (Step 4a), a translatability assessment was conducted by experienced translators in Hindi, Russian, and Spanish to assess the feasibility of translating the draft items into other languages for use in global studies.The measure was translated into additional languages. All translations underwent either full linguistic validation, including dual forward translations and dual backward translations or linguistics review. "(18)
10) What is the contribution of protein energy malnutrition to her severe hypoalbuminemia? What is the utility of tools such as SGA subjective global assessment in the evaluation of malnutrition in CRF patients?
Ans.
- In the setting of widespread chronic energy deficiency, BMI may not be a reliable marker of malnutrition. Anthropometric measurements such as skin fold thickness, mid arm circumference (MAC) and mid arm muscle circumference (MAMC) are widely used. However, the sensitivity of these methods in detecting early malnutrition, their practicability and their applicability to hemodialysis patients has not been convincing.
- It can detect the changing nutritional status which maybe missed by one time anthropometric and biochemical methods.
- It is a convenient bedside tool and can be used by paramedics as well.
2nd case
" A Danish study reported patients with diabetes mellitus were 3 times more likely to be hospitalized with pyelonephritis, as compared to subjects without diabetes"(19)
Any urinary tract obstruction could also lead to acute pyelonephritis, since he is a male, there could be obstruction due to an enlarged prostrate. (Another possible hypothesis causing acute pyelonephritis,which also seems likely as he is old)
Decline in urinary output since 3 days+ increase in serum creatinine+pH of blood is decreased with low partial pressure of CO2===> Acute kidney injury?
"Interstitial infiltration of neutrophils and phagocytes and extensive destruction of the parenchymal by the acute inflammatory process were found in AKI patients with acute pyelonephritis . These reports demonstrated that severe upper UTI might cause serious damage to the kidney and resulted in AKI."(20)
Even though both the pateints have Renal failure, this patient has an early stage renal failure.Whereas, in the 45 y/o woman's case she had developed full fledged ESRD and complications as well.
There is prolonged Aptt, thrombocytopenia and raised bilirubin which indicates some level of liver damage.
Differences in therapy:
nj.Piptaz 2.5mg/IV/TID---- to combat Urinary Tract Infection
Inj.Pantop 40mgIV OD
Inj.Lasix 40mg IV BD-- to relieve the low grade dema
Inj.HAI S/C according to sliding scale--for glucose levels control
Tab.Amlong 5mg OD----- Amlodipine to control the blood pressure
Strict I/O charting
GRBS charting 6th hrly
Bp charting 2nd hrly
Temp & pulse rate charting 4th hrly
Differences in outcome:
This patient has better prognosis than the previous patient as at this level if treated appropriately, the patient might not develop chronic kidney diease and complications.
2.Would you agree with the provisional diagnosis shared for this 58 M in the online case report linked above?
- Congenital small kidney
- Reflux nephropathy due to faulty drainage mechanism
- Renal artery stenosis
- Glomerulonephritis (usually effects both the kidneys but rare cases)
References:
1)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5656172/
2)
https://pubmed.ncbi.nlm.nih.gov/10207256/
3)
https://pmj.bmj.com/content/79/931/268
5)
https://acutecaretesting.org/en/journal-scans/should-bicarbonate-be-used-to-treat-metabolic-acidosis
6)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4549663/
7)
https://onlinelibrary.wiley.com/doi/full/10.1111/j.1524-6175.2004.4471.x#ss2-title
8)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5797340/
9)
https://www.hindawi.com/journals/bmri/2014/937398/
10)
https://cjasn.asnjournals.org/content/2/6/1186
11)
https://cjasn.asnjournals.org/content/1/2/193
12)
https://www.ahajournals.org/doi/10.1161/CIR.0000000000000691
13)
https://cjasn.asnjournals.org/content/1/2/193#ref-135
15)
https://pubmed.ncbi.nlm.nih.gov/16878035/
16)
https://imsear.searo.who.int/handle/123456789/182224
18)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7391458/#CR17
19)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4346284/








Comments
Post a Comment